L.A. Care Health Plan's Value Initiative for IPA Performance (VIIP) Programs offer performance-based incentives to participating Independent Practice Associations (IPAs). IPAs are incentivized for providing high-quality preventive and chronic care to L.A. Care members spanning multiple lines of business, including Medi-Cal, L.A. Care Covered (LACC) and L.A. Care Medicare Plus (HMO-DSNP).
Eligibility
There is no need to sign up for any of the VIIP Programs. IPAs are automatically enrolled and are eligible to earn incentive payments as long as they are contracted with L.A. Care and/or one of its sub-contracted Health Plans, including Anthem Blue Cross and Blue Shield of California Promise Health Plans.
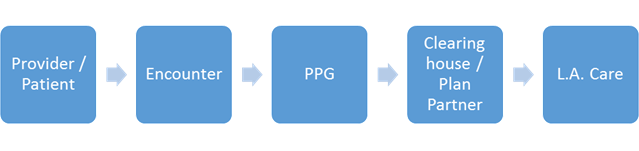
IPAs must also have L.A. Care members as of December 31st of the measurement year and must submit associated Encounter data, labs and care coordination and other supplemental sources through their usual reporting channels for it to count towards VIIP. For additional program rules, see the Program Description. To request a copy of the Program Description, contracted IPAs can contact us.
Data Submission Information
VIIP uses administrative HEDIS® data to determine incentive payments. Please review our HEDIS resources for more information. Data must be submitted via your usual reporting channels for it to be considered for VIIP.
Payments
Payments are remitted directly to the IPA unless otherwise specified (i.e. MSO). To make payments, L.A. Care must have a verified W-9 on file. It is the responsibility of each group to ensure that L.A. Care's VIIP staff is in possession of current and accurate W-9 information. If your tax ID or payment address changes or if you are unsure if the payment information on file is correct, please contact us to verify.